Dr. Mary Beth Madonna
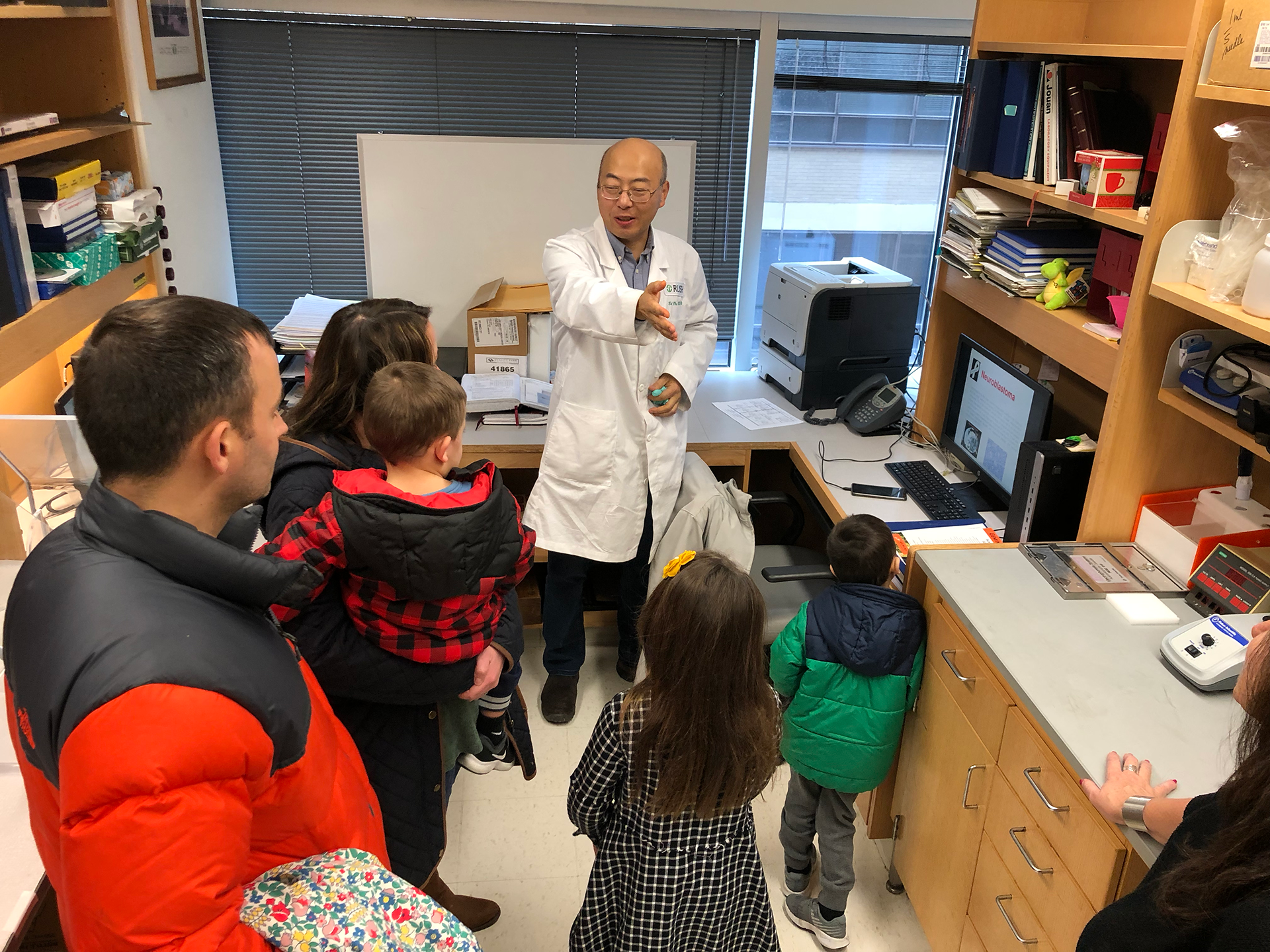
Neuroblastoma Pediatric Cancer Research
Dr. Madonna's research team has focused on studies to identify the basic biological processes that regulate adaptation of malignant tumor cells to stressful environments, such as those produced by anti-cancer drugs, and thereby permit their survival in the presence of agents that would normally kill them. Understanding these processes will help cancer researchers develop novel chemotherapeutic strategies.
Dr. Madonna’s team finds new avenues to discover better ways to treat neuroblastoma, the most common extracranial solid malignancy in infancy and childhood. Chemotherapy is the mainstay of treatment. Although initial chemotherapy helps eliminate neuroblastoma in a substantial number of affected children, the majority of neuroblastoma patients eventually develop progressive disease that is resistant to further therapy.
A deeper understanding of these processes will help cancer researchers develop novel chemotherapeutic strategies for the clinical setting.
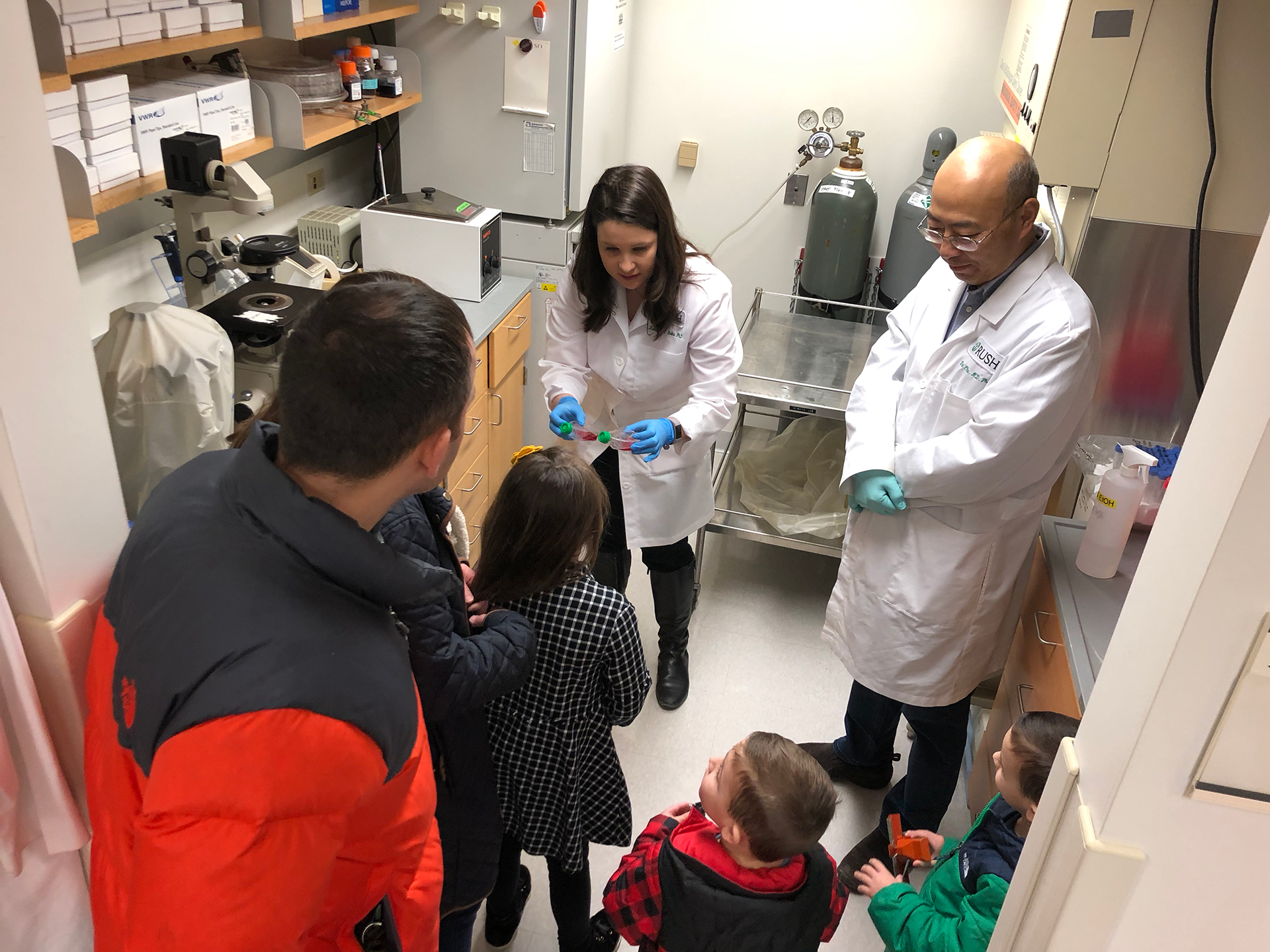
Dr. Madonna and her team have made considerable progress pursuing several different avenues of research, highlighted below, to reach the ultimate goal of finding new ways to screen for and effectively treat neuroblastoma.
Characterization of immune checkpoint expression in neuroblastoma
Cancer cells use checkpoint molecules to ‘turn off’ immune responses, thereby evading the immune system to survive. Checkpoint inhibitor immunotherapies activate immune cells to destroy cancer cells and thus may offer a novel therapeutic strategy for neuroblastoma patients. Currently, there are limited data available to help guide patient selection for immunotherapy to evaluate expected efficacy in neuroblastoma patients.
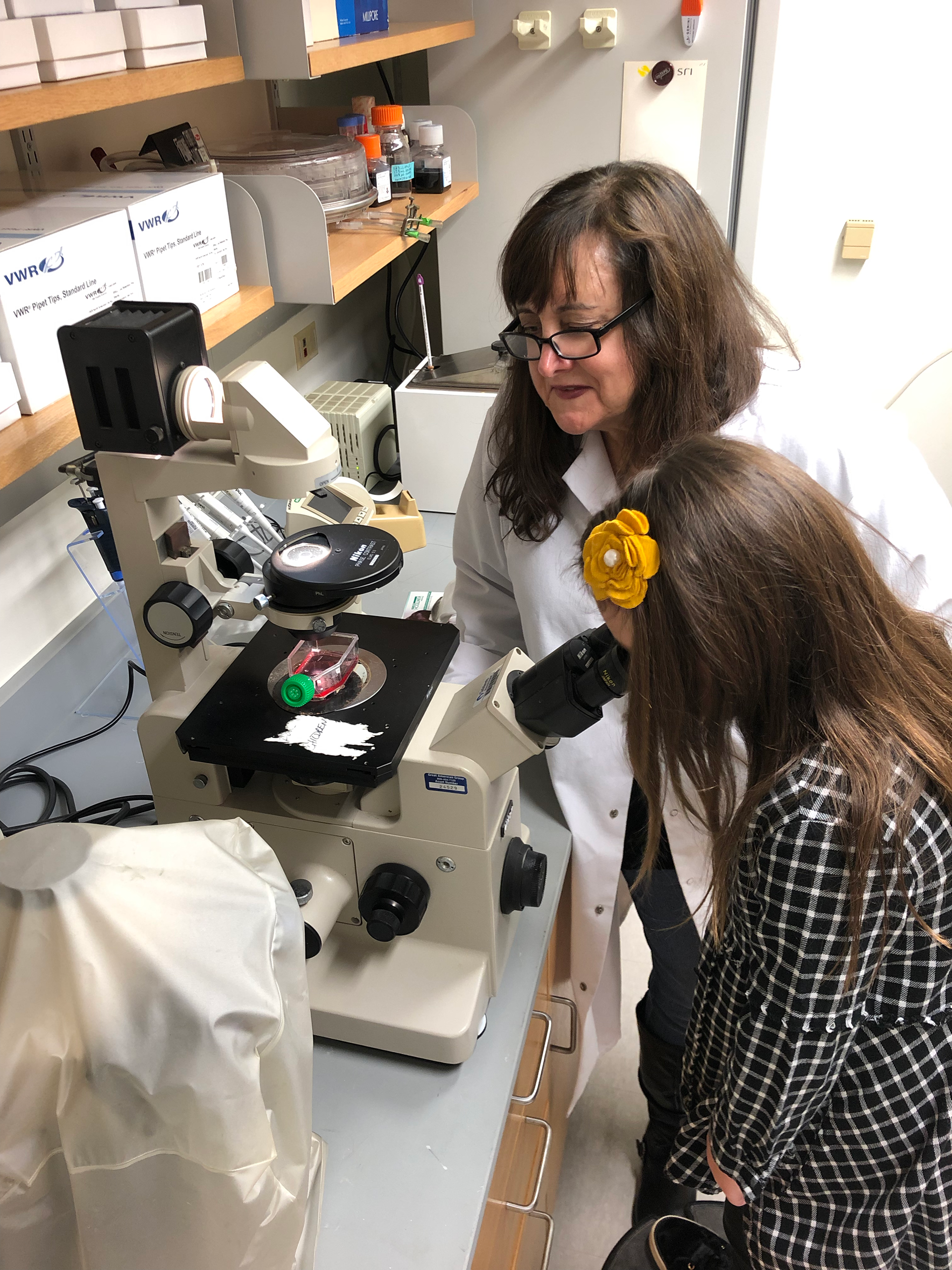
Dr. Madonna’s laboratory is uniquely situated to examine surplus tumor materials from patients due to RUSH’s strong clinical practice and banking of bio-specimens. Profiling immunomodulatory molecules is required to understand the immune system’s response to cancer, this will help illuminate immunotherapy’s role as a promising therapeutic approach for neuroblastoma.
Studying the role of hypoxia in the development of drug resistant in neuroblastoma
There is ample evidence that solid tumors frequently encounter hypoxic stress. Rapidly proliferating cancer cells may outgrow their vascular network, limiting O2 diffusion within the tumor. Importantly, hypoxia has been associated with drug resistance and reduced sensitivity to radiation therapy. Cellular response to hypoxia is controlled in part by hypoxia inducible factor-1α (HIF-1α). HIF-1α is recognized as a key modulator of the transcriptional response to hypoxic stress. Neuroblastoma often exhibits high levels of HIF-1α accumulation. Dr. Madonna’s team has found that hypoxia indeed plays a key role in the development of drug resistance, further research in this area may lead to new therapies that are able to overcome drug resistance to doxorubicin in clinical settings.
Elucidating the mechanism of action of the midkine signaling pathway in drug-resistant neuroblastoma
Expression of cytoprotective molecules such as the growth factor midkine is one of the drug-resistant mechanisms in neuroblastoma. Elucidation of the midkine signaling pathway could reveal novel therapeutic targets for treating drug-resistant neuroblastoma. Dr. Madonna’s lab was the first to report that midkine is secreted by drug-resistant neuroblastoma cells and induces the drug-resistant phenotype in neighboring drug-sensitive cells.
Furthermore, increased plasma midkine levels in neuroblastoma patients are significantly correlated with poor prognosis. The molecular mechanisms by which midkine induces the drug-resistant phenotype in drug-sensitive neuroblastoma cells are poorly understood. Identification of receptors directly interacting with midkine to induce drug resistance in neuroblastoma remains elusive. Dr. Madonna’s team seeks to elucidate the midkine signaling pathway in drug-resistant neuroblastoma, which could reveal novel therapeutic targets for treating drug-resistant neuroblastoma.
Targeting the Notch signaling pathway to overcome drug resistance in neuroblastoma cells
Dr. Madonna's work has suggested that Notch may serve as a receptor for midkine to exert its cytoprotective effects described above. There has been increasing evidence that targeting the Notch pathway could be a novel therapeutic approach for the treatment of cancer by overcoming drug resistance of cancer cells. This may lead to the elimination of cancer stem cells, which are typically drug-resistant and are believed to be the “root cause” of tumor recurrence. Dr. Madonna’s lab found that Notch inhibitor synergized with doxorubicin, reducing the cell viability of drug-resistant neuroblastoma cells by 63%. Modifying the Notch signaling pathway could be a promising approach for dealing with drug resistant neuroblastoma and may have a great clinical significance.